Microsoft Office 2007 Enterprise Activated And Tested Negative For Herpes
Results Median HSV shedding episode duration was 7.5 (range 4–253) hours for oral and 11 (range 4–328) hours for anogenital reactivation. Thirty-five percent of oral and 29% of anogenital reactivations lasted ≤ 6 hours, and 59% of oral and 53% of anogenital reactivations lasted ≤ 12 hours. Seven of 9 participants who shed orally and 10 of 15 who shed anogenitally had ≥ 1 reactivation lasting ≤ 6 hours. The median maximum level of HSV DNA detected in an episode increased with episode duration for both oral and anogenital episodes. Concurrent oral and anogenital shedding occurred more frequently than expected: Oral HSV shedding was detected on 17% of time points with anogenital, but 1% of time points without anogenital, shedding (p. Introduction Chronic HSV ulcers were one of the first described manifestations of AIDS, and HIV-infected persons have higher clinical anogenital HSV recurrence rates, higher anogenital HSV-2 shedding rates,, and higher oral HSV shedding rates than HIV uninfected persons. Higher rates of both HSV shedding and HSV clinical recurrences among HIV-infected persons compared with HIV uninfected persons are presumed to be caused by decreased host ability to control HSV replication.
RebelMouse is the best CMS 2017 and #1 Wordpress VIP alternative. See what makes us so fast, and why you should re-platform with us today. Feb 23, 2017. 4.5 PDGFRα-dependent entry ans PDGFRα activation. Shown that only gH/gL/gO-positive HCMV infects cells in a PDGFRα-dependent manner: i). Microsoft Office (Excel, Powerpoint, Word). BD Biosciences. GraphPad Prism 5. GraphPad Software.
However, there is considerable variability in HSV-2 reactivation rates in HIV-infected, as in HIV-uninfected, persons, even among those with similar CD4 T cell counts. In general, severe persistent HSV-2 genital ulcer disease has been associated with CD4 T cell counts. Study participants and procedures HSV-2 seropositive, HIV-1 seropositive participants aged ≥ 18 years were recruited in 2006–2007 from a pool of prior research study participants known to be able to comply with an intensive study protocol and asked to collect oral and anogenital swab specimens for HSV DNA PCR at home 4 times per day for 60 days. Swab specimens were collected at ∼6 hour intervals: upon awakening, in the midmorning, in the afternoon, and at bedtime. Participants recorded in a diary exact swabbing times and any symptoms present, and were instructed not to take any herpes antiviral medication during the study. As previously described,,,, anogenital swabs were obtained by rubbing a polyester fiber-tipped swab across first the penile and then the perianal skin for men, or first across the posterior cervical/vaginal, then vulvar, then perianal areas for women. Oral swabs were performed by rubbing one swab across the buccal mucosa and tongue.
Separate swabs were collected from any oral or anogenital lesions noted by the participant. Participants were seen in the clinic every 3 weeks for collection of samples and diary review. Blood was drawn for both CD4 T cell count and serum HIV-1 RNA level within one month of starting the swabbing study, and antiretroviral use was obtained by history at the time of study initiation. Highly active antiretroviral therapy (HAART) use was defined as receipt of at least 3 drugs in 2 of the following categories: protease inhibitor, nucleoside analogue, or non-nucleoside analogue, at the time of study initiation. This study was approved by the University of Washington institutional review board, and all participants gave written informed consent. Laboratory methods HIV-1 seropositivity was confirmed by standard enzyme-linked immunoassay and Western blot. HSV serologic testing was performed by Western blot.
Absolute CD4 T cell counts were determined by flow cytometry. HIV-1 RNA levels were measured using real-time RT PCR technology (detection level, 30 HIV-1 RNA copies per mL). Oral, anogenital, and lesion swabs were placed into separate vials containing 1 mL of PCR transport medium and stored at -20°C until laboratory processing.
HSV DNA was detected using a quantitative real-time PCR assay and expressed as copies per mL of transport medium., As previously described, the initial PCR assay uses type-common primers to the HSV glycoprotein B gene, with positive samples subsequently analyzed using type-specific primers to determine whether DNA detected was that of HSV-1, HSV-2, or both., An internal control was included in the PCR reaction to ensure that HSV-negative findings were not due to inhibition. Samples were considered positive for HSV if we detected ≥ 3 copies of HSV DNA per 20 μL of specimen (i.e., ≥ 150 copies of HSV DNA per mL of transport media). Laboratory personnel were blinded to clinical data. Statistical analysis Analyses were done using SAS (SAS Institute Inc, Cary, North Carolina). We used identical definitions of HSV shedding, shedding rate, and shedding episode as in our previous work examining shedding in immunocompetent adults. Briefly, HSV shedding was considered to have occurred if an oral or anogenital sample or the corresponding lesion sample was positive for HSV at a given time.
If both the oral or anogenital sample and the corresponding lesion sample were positive for HSV, the sample with the higher HSV DNA copy number was used in further analyses. Idmgcext Crx 6 23 Download Mp3. Shedding rates were defined as number of swab specimens with HSV DNA detected divided by number of swab specimens collected. Number of days with samples collected was defined as total days from first to last day of specimen collection for both oral and anogenital samples, minus any days during which no samples were collected; expected number of days per participant was at least 60. Rengou Vs Zaft 2 Plus Isotopes. On each day with any genital (or oral) sampling done, 4 genital (or oral) swabs were expected. A shedding episode of known duration was defined as one or a series of HSV-positive swab specimens that were collected immediately before and after at least 2 HSV-negative swab specimens.
Episode start time was estimated as the chronological midpoint between the last HSV-negative and first HSV-positive swab specimen, and episode stop time as the midpoint between the last HSV-positive and first HSV-negative swab specimen. Since not all time points had swab specimens available, some subjects shed HSV for an unknown period. These are referred to as shedding episodes of uncertain duration, because the episodes may have been longer than observed. For these episodes we assumed missing swab specimens 2 time points before and 2 time points after the positive swab specimen(s) were HSV negative and estimated start and stop times as above. Any shedding episode (of known or uncertain duration) could include 1 missing or 1 HSV-negative swab specimen within the episode. Generalized estimating equations were used to determine whether there was a difference in average episode duration between episodes of known and uncertain duration, whether there was an association between average per-episode maximum HSV DNA copy number and episode duration, and whether concurrent oral and anogenital shedding occurs more frequently than would be expected by chance alone. Wilcoxon rank sum tests were used to test for differences in median CD4 count and HIV viral load among persons taking and not taking HAART and to examine person-level differences in shedding rates and number of reactivations by anatomic site.
Fisher's exact test was used to test for associations between episode length and anogenital symptoms and lesions. Generalized estimating equations were also used to examine associations between measures of HIV disease severity (CD4 count, HIV viral load, and HAART use) and duration of or maximum HSV copy number in shedding episodes. CD4 count was dichotomized at 200 cells/mm 3 and HIV viral load at 10,000 copies/mL based on prior studies indicating this degree of immunosuppression and HIV viral replication were associated with longer HSV shedding duration. Study population Twenty participants collected oral and anogenital samples for a median of 62 (range 32-79) days, with 20 (100%) participants collecting samples for at least 30 days, 18 (90%) for at least 50 days, and 15 (75%) for at least 60 days.
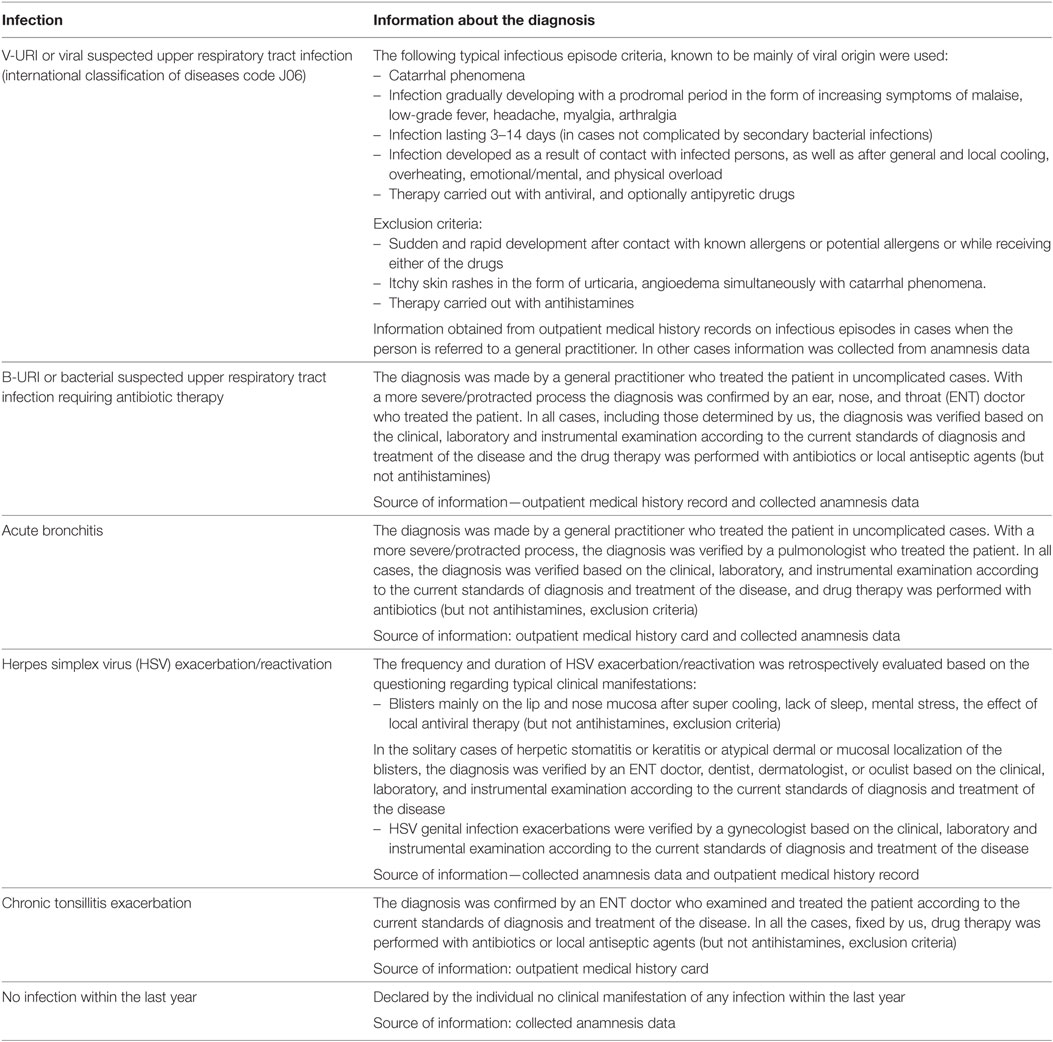
Participants, who included 19 men and 1 woman, had a median CD4 count of 426 (range 29-1066) cells/mm 3, and a median HIV-1 RNA level of 2280 (range. Frequency of mucosal HSV shedding Oral samples were collected for 1201 days (95% of the expected 1269 days) and 4559 time points (95% of the expected 4804 time points), and anogenital samples for 1199 days (94% of the expected 1269 days) and 4544 time points (95% of the expected 4796 time points). Both oral and anogenital samples were collected at all 4 time points on 87% of days and at 3 of 4 time points on 7% of days, thus 94% of days had at least 3 daily oral and anogenital samples collected. HSV DNA was detected from oral samples on 58 (5%) days and 120 (3%) time points and from anogenital samples on 199 (16%) days and 535 (12%) time points (p = 0.002, indicating more frequent anogenital than oral shedding; see ). Nine (45%) participants had at least one oral sample in which HSV was detected and 15 (75%) at least one anogenital sample in which HSV was detected. Proportion of days, time points, and participants with HSV detected in at least 1 sample, and HSV typing. Duration of HSV reactivation as defined by 4 times daily sampling is shown for 29 oral and 66 anogenital shedding episodes of known duration.
HSV typing was available for 109 (91%) of 120 oral samples and 533 (99.6%) of 535 anogenital samples; the copy number in the remaining samples was too low for typing. Number and duration of shedding episodes We identified 36 separate episodes of oral HSV shedding in 9 participants and 82 episodes of anogenital HSV shedding in 15 participants. Complete 4 times daily sampling allowed calculation of oral shedding duration for 29 (81%) episodes and anogenital shedding duration for 66 (80%) episodes. The median duration of an oral HSV reactivation with complete sampling was 8 hours (range 4 hours – 11 days) and an anogenital reactivation with complete sampling, 11 hours (range 4 hours–14 days) (). Of the 29 oral episodes of known duration, 10 (34%) lasted ≤ 6 hours, 17 (58%) lasted ≤ 12 hours and 19 (66%) lasted ≤ 18 hours (). No oral shedding episodes of known duration consisted of sole HSV-1 shedding; 17 (59%) were HSV-2 oral shedding episodes (median duration 12 [range 5-36] hours), 6 (21%) included both HSV-1 and HSV-2 shedding (median duration 34 [range 6-253] hours), and 6 (21%) could not be typed (median duration 6 [range 4-8] hours).
Of the 66 anogenital shedding episodes of known duration, 19 (29%) lasted ≤ 6 hours, 35 (53%) lasted ≤ 12 hours and 43 (65%) lasted ≤ 18 hours. Sixty-three (95%) contained HSV-2 only, 2 both HSV-1 and HSV-2, and 1 could not be typed (). The median maximum copy number of HSV DNA detected during both oral and anogenital episodes increased with episode duration (for episodes lasting ≤ 24 hours and >24 hours 10 2.9 versus 10 4.7 copies orally, p = 0.009, and 10 3.3 versus 10 4.9 copies anogenitally, p.
Herpes simplex virus (HSV) shedding episode duration and viral copy number, of 29 oral and 66 anogenital shedding episodes of known duration. (A) Oral and (B) anogenital episode duration and (C) oral and (D) anogenital HSV copy number by episode duration.
The median number of HSV reactivations of known duration among those who shed during the 60 day sampling period was 3 (range 1–8) oral and 4 (range 1–18) anogenital reactivations per person. Excluding the 11 participants who were not observed to shed orally, the median oral HSV reactivation rate was 1.4 (range 0.4–9.5) reactivations per 30 days or 16 reactivations annually. Excluding the 5 participants who did not shed anogenitally, the median anogenital HSV reactivation rate was 2.1 (range 0.5–8.6) reactivations per 30 days or 26 reactivations annually (p = 0.17 for comparison between oral and anogenital reactivation rates).
Associations Between Shedding and Symptoms No oral HSV reactivation was accompanied by symptoms or lesions. Three (5%) of 63 anogenital episodes of known duration with symptom and lesion information were associated with lesions and 5 (8%) with symptoms. Shorter anogenital shedding episodes were less likely to be symptomatic than longer ones. None of 45 anogenital shedding episodes lasting ≤ 24 hours had lesions, compared with 3 of 21 (14%) anogenital episodes >24 hours (p = 0.029).
Similarly, only 1 of 45 (2%) anogenital episodes lasting ≤ 24 hours was associated with symptoms, compared with 4 of 21 (19%) anogenital episodes >24 hours (p = 0.032). Concurrent Oral and Anogenital Shedding Swab samples were collected concurrently from both oral and anogenital sites at 4499 time points, with HSV detected on both oral and anogenital swabs concurrently at 89 time points. Concurrent shedding occurred in 4 participants (shedding data from 2 of these 4 are shown in ) and occurred more frequently than would be expected by chance alone: oral HSV shedding was detected on 17% (89/532) of time points when HSV was detected anogenitally but on only 1% (30/3967) of time points when anogenital shedding was not occurring (p. Effect of immune status on HSV shedding In our population, CD4 count, HIV viral load, and antiretroviral use did not affect the duration of HSV shedding episodes (the proportion of episodes ≤ 6 hours versus >6 hours, ). However, univariate analyses showed both antiretroviral use and a plasma HIV RNA.
Discussion Our study indicates that oral and anogenital HSV-1 and HSV-2 reactivation are even more common in HIV-infected persons than previously appreciated. In particular, subclinical oral shedding of HSV-1 and HSV-2 is quite common. Most mucosal HSV reactivations in HIV-infected persons are short and subclinical, with a median anogential HSV reactivation duration of 11 hours. Twenty-nine percent of anogenital HSV reactivations last ≤ 6 hours and over half (53%) last ≤ 12 hours.
We also found that concurrent oral and anogenital HSV shedding, often of the same viral type but sometimes of different viral type, occurred more frequently than would be predicted by chance, supporting the findings of Kim et al. It is of interest that simultaneous reactivation from oral and anogenital mucosa, often with different subtypes, happens more frequently than would be predicted to occur, suggesting common systemic or mucosal host factors influencing shedding. Interestingly, oral HSV-2 shedding was as common as oral HSV-1 shedding; among HSV-1/HSV-2 seropositive participants, 46% of oral samples showed HSV-1 alone and 43% showed HSV-2 alone. We do not know whether oral HSV-2 shedding during episodes of oral-genital contact with a HSV-2 negative partner can lead to partner acquisition of genital HSV-2 infection, but this is certainly biologically plausible.
These data on HSV reactivation duration in HIV-infected persons are similar to what we found in immunocompetent hosts, who had a median anogenital HSV reactivation duration of 13 hours, with 24% of reactivations lasting ≤ 6 hours and 49% lasting ≤ 12 hours. We studied an HIV-infected population that was only moderately immunosuppressed (median CD4 count 426 cells/mm 3) and our results may have been different if we had enrolled only HIV-infected persons with more marked immunosuppression (CD4.
